
Genital discharge in men is a discharge from the urethra and secretions of the preputial glands, which are located on the head of the penis, under the skin of the foreskin. The ejaculatory duct, prostate ducts, urethral and bulbourethral glands open into the urethra.
In a healthy man, only urine and ejaculate flow through the urethra. This is a physiological discharge from the penis and should not cause discomfort. Unfortunately, this is not always the case.
For various reasons, men's health is shaken and instead of a normal discharge, an abnormal discharge appears or urine and semen change
Variants of physiological secretions
Criteria for normal discharge corresponding to the functions of the organs of the urogenital system:
- Urine - clear, from straw to golden-yellow color, practically odorless, does not contain flakes or other inclusions;
- The secretion of the prostate has a viscous consistency and whitish hue, there is a specific smell of sperm;
- Ejaculate: semen from the ejaculatory canal mixes with secretions of Littre's glands (urethral), Cooper's (bulbourethral) and prostate, obtaining a grayish-white color and consistency of mucus;
- Fresh smegma from the preputial glands is like a thick white fat; it may become yellowish or greenish over time.
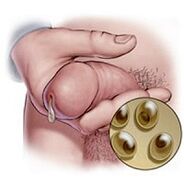
The preputial lubricant - smegma - is constantly released, accumulating under the inner layer of the foreskin and in the coronal groove of the penis. The lubricant consists of fat and bacterial residues, is evenly distributed and reduces friction between the skin of the foreskin and the scalp. The maximum activity of the preputial glands is characteristic of the period of puberty, with age the secretion decreases and completely stops until old age.
If you ignore the rules of personal hygiene, smegma can accumulate under the folds of the skin. In this case, the fatty part of the lubricant oxidizes, and the protein part decomposes (in fact, rots), and the masses become greenish, taking on an unpleasant odor. The same process occurs with phimosis, when due to the joining of the foreskin, it is impossible to completely free the head of the penis from skin folds and remove smegma. Accumulation and degradation of lubricants can lead to chronic balanitis and balanoposthitis (inflammation of the skin and glans penis), increasing the risk of tumor development.
Urethrorea, mucous, colorless discharge from the bulbourethral and urethral glands. Discharge data appear in men with libido-related arousal. The secretion of clear mucus aims to lubricate the urethra and improve the passage of semen. The amount of secretion ranges from scarce to abundant, these parameters are related to the individual characteristics of the organism and the frequency of sexual activity. After prolonged abstinence, the volume of secretions increases.
Pollution is the spontaneous release of sperm, which is not related to intercourse. It is usually seen in the morning when testosterone levels rise. It depends on the age and intensity of sexual activity: it occurs in boys at puberty, in adult men - in irregular or infrequent intercourse.
Prostatory, discharge from the urethra of a small amount of clear mucus with grayish-white inclusions. It occurs after tension in the abdominal muscles (for example, in constipation) or after urination. The secretion consists of a mixture of sperm and prostate discharge, increased volume and opacity may be signs of prostatitis.
Pathological discharge
In men, the causes of penile discharge can be sexually transmitted diseases, tumors, nonspecific inflammation of the urogenital organs, various injuries, medical manipulations or surgery.
Pathological discharge from the urethra differs from normal:
- By volume (too abundant or small, possibly moderate);
- By color and transparency (from white to yellow-green, dull);
- Impurities (blood, pus, lumps of mucus);
- Consistencies (very sparse or too thick and sticky);
- By smell (sour, rotten, fishy);
- By frequency of occurrence (depending on the time of day, constant or episodic discharge);
- Regarding urination, sexual arousal, alcohol intake, spicy and spicy foods.
The nature of the discharge depends on the cause of the disease, the status of the immune system, the accompanying problems, as well as the severity and duration of inflammation (acute or chronic).
If the amount, density or color of the discharge changes, if an unpleasant odor appears, it is recommended to consult a doctor and have an examination. Self-diagnosis is not worth it, it is very difficult to correctly recognize the disease by just one symptom.
Penile discharge associated with sexually transmitted diseases
Mucus: clear discharge, viscous and small amounts, found in the chronic form of chlamydia, mycoplasma or ureaplasma urethritis. Microscopically, a moderate number of leukocytes in the secretion is detected (the norm is up to 4 cells per visual field).
Mucopurulent: white discharge, transparent; observed in the exacerbation phase with chlamydia, ureaplasmosis, and mycoplasmosis. In chlamydial infections, they accumulate on the head of the penis, as if "sticking" to the skin.
In the pathologies described above, the discharge will come from the urethra itself, because microorganisms irritate the mucous membrane of the urethra, and the body tries to "wash" it.
It happens that the secret of white color seems to cover the head. This is noted in chlamydia, candidiasis. In the first case, a film is formed, in the second - a loose cheesy inflorescence.
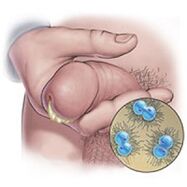
A purulent discharge with an unpleasant odor is characteristic of gonorrhea. They are sticky, thick, yellow or greenish in color, rotten in smell. Microscopic examination of the material shows epithelial cells from the urethra, many leukocytes.
Symptoms accompanying gonorrheal urethritis: persistent and profuse discharge; pain, itching and tingling are especially strong when urinating.
In sexually transmitted diseases, combined infections that combine several pathogens at once are often observed. Gonorrhea and trichomoniasis are accompanied by chlamydia, mycoplasmosis and ureaplasmosis are usually found in pairs. The symptomatology of such diseases differs from the classical manifestations, the discharge from the urethra can also acquire a completely different character. Therefore, modern analytical techniques with a high degree of reliability are used for the final diagnosis, and not the characteristics of the discharge.
Nonspecific (non-venereal) inflammation
The cause of non-specific inflammation is its own microflora, which is conditionally pathogenic and is activated only in the case of problems with the body's immune defense. Streptococci and staphylococci, fungi of the genus Candida and E. coli are always present on the surface of the skin and mucous membranes, but begin to actively multiply and displace beneficial bacteria after hypothermia, long-term stress, uncontrolled antibiotic treatment, radiation and chemotherapy.
Non-gonorrheal (nonspecific) urethritis. Inflammatory discharge is small in volume, visible in the urine as mucopurulent bands or lumps, which appear at the very beginning of the disease. Symptoms such as tingling and itching when urinating are less pronounced than with gonorrhea, but the urge is common and does not bring relief. With ascending infection, the bladder becomes inflamed first, followed by the ureters and kidneys; a discharge with an admixture of crimson blood appears.

Candidiasis (thrush), a fungal infection of the urethra. It usually develops against the background of suppression of the immune system after a course of antibiotics, chemotherapy or radiotherapy; sexual transmission of candidiasis in men is rare. Thrush is characterized by a clotted discharge with a sour smell, which is combined with itching and burning during urination (urination) and ejaculation (ejaculation), and can be accompanied by dull pain in the groin, above the pubis and in the lower back.
Gardnerellosis of the urethra. The fishy smell of the discharge is characteristic; they are sparse, yellowish white or greenish. According to some classifications, gardnerellosis is called a sexually transmitted disease, but in men, sexual gardnerella infection is more likely to be a curiosity. In fact, this disease is associated with a violation of the normal microflora, or dysbiosis. Immunocorrectors and probiotics (lactic acid bacteria) must be used in its treatment.
Balanoposthitis, inflammation of the foreskin. Abundant purulent discharge is observed locally, a mixture of mucus is possible. Always accompanied by edema and hyperemia (redness) of the foreskin leaves, pain in the head of the penis.
In prostatitis, at the end of urination there is a cloudy discharge, copious discharge - in the acute period of inflammation; sparse and white - with the transition of the disease to a chronic form. Prostatitis is usually complicated by difficulty urinating and poor erection, in severe cases - to anuria (complete absence of urine flow) and impotence.
Discharge is not associated with inflammation

Spermatorrhea - a discharge in the form of passively flowing sperm, occurs outside of sexual intercourse or masturbation, without a feeling of orgasm. The reasons are some diseases of the nervous system, spinal injuries, chronic stress and any prolonged inflammation of the genital area. Spermatorrhea is associated with a violation of innervation and a decrease in vas deferens tone.
Hematorrhea, spots. It often occurs with urethral canal injuries sustained during cuffing, after catheter insertion, or when taking a swab from the mucosa. In these cases, the blood is fresh, without clots, a small amount, the bleeding stops quickly. When small kidney stones or sand disappear, blood is released during or immediately after urination, hematorrhea is accompanied by very severe pain (renal colic). Blood discharge in the hematuric form of glomerulonephritis (inflammation of the renal glomeruli) is combined with edema and constant high blood pressure, the appearance of protein in the urine.
A brown discharge, with clots of blood or mucus, mixed with pus, occurs in malignant tumors that come out of the prostate, urethra, or bladder. Brownish mucus can form during the healing of wounds on the mucous membranes, and is secreted by polyps of the urethra and / or bladder.
Prostatitis is the secretion of the prostate that flows from the urethra. It occurs in chronic prostatitis, prostate adenoma, disturbed innervation (neurogenic bladder).
Examination algorithm in the presence of pathological discharge from the penis

- Examination of the perineum, penis, foreskin and glans. The goal is to identify deformities of the genital organs, traces of their injury, signs of external inflammation, discharge, rash, etc. Traces of discharge are sometimes visible on the bedding.
- Palpation of inguinal lymph nodes, assessment of their condition: size, they are warmer or colder than the surrounding tissues, painful or not, soft or dense, mobile or sticky to the skin, whether there are ulcerations above them.
- Finger examination of the prostate; massaging the prostate through the rectum and taking secretions for microscopic examination. Before the massage, it is recommended to refrain from urinating for 1-2 hours. In the case of prostate adenoma, its lobes are enlarged approximately equally, dense strands are felt. Uneven growths and their consistency are typical for malignant tumors; on palpation of the prostate, blood with clots may be released from the urethra.
- Material - smears for microscopy and culture. When examined under a microscope, the stained smear shows blood cells, epithelium, sperm, fat inclusions, some pathogens (Escherichia coli, gonococci, gardnerella, yeast). An increased number of leukocytes is characteristic of acute urethritis or exacerbation of chronic inflammation, eosinophils - for urethritis with allergies. Erythrocytes are found in severe inflammation, tumors, injuries of the genitourinary organs, urolithiasis. A large amount of epithelium is a sign of chronic urethritis, urethral leukoplakia. In spermatorrhea, sperm are in the smear, in the urethra - mucus, prostate - lipid granules. For informative content and reliability of results, the swab is taken no later than 3 days after local application of antibiotics, antifungals and disinfectants. If antibiotic therapy was systemic, it should be at least 3 weeks after the course. Do not wash before taking the swab, try not to urinate for 2-3 hours.
- General clinical analysis of blood, blood sugar - in the morning, on an empty stomach. Extended urine analysis (morning, immediately after sleep).
- Ultrasound of the prostate, bladder and kidneys; CT and urography.
If the manifestations of genital inflammation are strong, then before the test results are obtained, the patient is immediately prescribed broad-spectrum antibiotics. In case of heavy bleeding, hospitalization and active measures to stop the bleeding are indicated. Confirmation of the suspicion of a malignant tumor can only be the result of a biopsy, the final diagnosis is made on the basis of histological examination.
Important:
- Penile discharge is just one of the symptoms that cannot be taken into account when making a diagnosis.
- Independent farm naming is unacceptable. medications, even if they appear obvious for a particular disease.

































